Adult Sleep Apnea Treatment
In the United States alone, millions of people suffer from undiagnosed sleep apnea and they experience the problems this disorder causes. Millions more have been diagnosed with this disorder but have no solution that puts an end to it. They may rely on routine oral appliances they have to wear for the rest of their lives. Or they are subjected to an intrusive face mask (CPAP machine) that sends continuous air pressure to the throat to enable them to breathe at night. This mask can be so uncomfortable that it causes most patients to abandon using it.
Some people submit to a surgery that reshapes the bones of the face or jaws or that trims tissues in the throat, all in an attempt to improve nighttime airflow and obtain quality sleep.
It’s easy to understand their desperation. The list of problems created by sleep apnea go far beyond the snoring and gasping it causes:
Long-term Effects
- Memory loss
- Chronic fatigue
- Depression
- Mental confusion
- Weakened immunity
- High blood pressure
- Increased risk for stroke or heart attack
- Increased risk of dementia
- Irregular heart rhythm
- Diabetes
Short-term Effects
- Waking up unrefreshed
- Dry mouth from breathing through the mouth
- Fatigue
- Daytime sleepiness
- Headaches
- Irritability
"I have been a Vivos patient under the care of Dr. Seifi for almost 10 months. Dr. Seifi's Team and practice are very professional. I was having problems with my bite, mouth/jaw mechanics and night breathing after my previous orthodontics treatment. I was introduced to the Vivos appliance. After further assessment, I decided to give it a try. So far, I've seen great improvements in my breathing at night (able to sleep on my back all night), my mouth/jaws are more relaxed, no more biting of my cheek, less headaches and my speech is clearer. And I'm happy to see my wide smile again!"
- M. R.
It’s clear that sleep apnea is more than just snoring—this is one of the sleep disorders that can have the biggest impact on your quality of life. Do you suffer from sleep apnea? Are your symptoms becoming overwhelming? Do you wonder if there are better options for sleep apnea treatment? Properly treating sleep apnea will improve your overall health and give you a better night’s sleep. Before you can receive treatment, however, you must understand how this condition works and undergo diagnostic testing with a doctor.
What Is Sleep Apnea?
Sleep apnea is a condition where your breathing stops and starts over and over while you’re asleep. There are different types of sleep apnea and each condition works slightly differently
Sleep apnea has a longer history than you might think. It was originally called Pickwickian syndrome based on the condition mentioned in
The Pickwick Papers
by Charles Dickens. Medical literature did not refer to sleep apnea until 1965. The first CPAP was developed in 1981 and researchers continue to study sleep apnea and the best methods of treating it today.
This is one of the most common sleep disorders, affecting
22 million people in the U.S. However, it can also be dangerous, especially when undiagnosed. If sleep apnea is not treated, it can lead to life-threatening medical conditions such as chronic heart failure, stroke, or other cardiovascular issues. And if you’re drowsy during the day while driving, you could cause a traffic accident.
Data published in the American Journal of Epidemiology indicates that obstructive sleep apnea is
becoming even more common. Prevalence rates of this condition have significantly increased over the last two decades. This is most likely because of the obesity epidemic, as obesity increases the chances of sleep apnea. The data published in the journal estimates that 26% of adults between 30-70 years old have sleep apnea.
Types of Sleep Apnea
There are three types of sleep apnea:
- Obstructive Sleep Apnea
- Central Sleep Apnea
- Complex Sleep Apnea
Obstructive and central sleep apnea are two distinct conditions with different mechanisms. Complex sleep apnea is a combination of the first two conditions.
Obstructive Sleep Apnea
With
obstructive sleep apnea, the muscles in your throat relax and block your airway during sleep. The muscles in the back of your throat support your:
- Soft palate (the back of the roof of your mouth)
- Uvula (tissue that hangs from the soft palate)
- Tonsils
- Tongue
If those throat muscles relax too much, your airway narrows or even closes completely. Your tongue also relaxes while you’re asleep and
might fall back into your airway. This interrupts your breathing and lowers the oxygen level of your blood. For people who have obstructive sleep apnea, their brain wakes them up multiple times a night so they can breathe.
Obstructive sleep apnea is the most common type of sleep apnea. This condition is measured using something called the
apnea-hypopnea index (AHI), which tracks how many times you stop breathing or breathe shallowly while asleep. This allows doctors to categorize patients into the following groups:
- Severe obstructive sleep apnea. If your AHI is greater than 30 (meaning you have more than 30 episodes per hour), you have severe obstructive sleep apnea.
- Moderate obstructive sleep apnea. An AHI between 15-30 results in this diagnosis.
- Mild obstructive sleep apnea. Mild obstructive sleep apnea comes with an AHI of 5-15.
Central Sleep Apnea
If you have
central sleep apnea, your brain doesn’t transmit signals to your breathing muscles correctly. Some types of central sleep apnea are connected with congestive heart failure or stroke. Others have to do with medications—like opioids or codeine. Still others may happen if you are sleeping at a high altitude.
Central sleep apnea comes from a lack of respiratory effort during sleep. When you breathe in, your brain sends a signal to your diaphragm and the muscles of your rib cage so they will contract. In central sleep apnea, this communication between brain and muscles is dysfunctional. This condition is different from obstructive sleep apnea, where a person is trying to breathe but cannot due to airway blockage.
One type of central sleep apnea is the hypoventilation type, where the brain doesn’t send signals to the respiratory muscle. Another type is hyperventilation alternating with pauses in breathing.
Complex Sleep Apnea
Complex sleep apnea is the term used for somebody who has both obstructive sleep apnea
and
central sleep apnea. This can also be called
mixed sleep apnea.
For example, some people who have obstructive sleep apnea and use a CPAP to treat it end up developing central sleep apnea, too. This is called treatment-emergent central sleep apnea.
Symptoms of Sleep Apnea
The symptoms of obstructive sleep apnea and central sleep apnea vary slightly. Obstructive sleep apnea symptoms in adults include:
- Excessive daytime sleepiness; frequently falling asleep while doing other activities
- Trouble concentrating or remembering things
- Loud snoring
- Snoring interrupted with periods of quiet
- Waking up gasping or choking
- Waking up with a dry mouth or sore throat
- Morning headache
- Depression or irritability
- Episodes of not breathing while asleep (as observed by a partner or family member)
- High blood pressure
- Decreased libido
Symptoms of central sleep apnea can be:
- Daytime drowsiness
- Morning headaches
- Trouble concentrating or remembering things
- Inability to exercise like usual
- Waking up often during the night
- Mood changes
- Insomnia
- Abnormal breathing patterns while asleep (as observed by a partner or family member
Unlike obstructive sleep apnea, snoring is not a common symptom for central sleep apnea.
When to See a Doctor
Just because you snore while asleep doesn’t necessarily mean you have sleep apnea. Snoring
can also be caused by sinus issues, sleep deprivation, or drinking alcohol before bed. However, snoring combined with certain other symptoms may be cause for concern. You should speak with a doctor about your symptoms if you are experiencing:
- Snoring that’s so loud it disturbs your sleep
- Morning headaches
- Excessive daytime drowsiness (falling asleep while working, driving, or watching TV)
- Breathing pauses while you’re asleep
- Waking up gasping or choking
- Problems concentrating during the day
A
These symptoms should be reviewed by a medical professional.
Causes of Sleep Apnea
There are multiple causes of sleep apnea in adults. Obstructive sleep apnea is
most commonly caused by obesity or excess weight. A larger neck circumference than average is associated with sleep apnea. Over half of people who have obstructive sleep apnea are overweight or obese, and a weight gain of just 10% increases your risk of obstructive sleep apnea by six times.
Obstructive sleep apnea could also be caused by:
- A narrow throat
- Allergies
- Deviated septum or nasal congestion
- Smoking (people who smoke cigarettes are at a
higher risk for sleep-disordered breathing)
- Alcohol or drug abuse
- A round head
- Hypothyroidism or other hormonal conditions
- Family history
- Certain medications (including opiates or sedative drugs)
When it comes to central sleep apnea, doctors are often unable to determine the exact cause. However, central sleep apnea might be caused by another medical condition (such as heart failure or kidney problems). Medications such as opiates can also cause central sleep apnea. And if you’re sleeping above 15,000 feet, you may experience central sleep apnea until you come back to a lower altitude.
In some cases, you may be able to reduce your risk of developing sleep apnea. You can’t control your anatomical characteristics—how your neck, jaw, tongue, and tonsils are positioned. But you can avoid smoking and avoid drinking excess alcohol. If a doctor has advised you to lose weight, this will be helpful, too. Sleeping on your back also makes it easier for your airway to become blocked.
Sleep Apnea Complications
If sleep apnea is not treated properly, it can lead to serious health complications. Studies have indicated that sleep apnea
can cause issues like type 2 diabetes, stroke, heart attacks, and a short lifespan. Over time, sleep apnea can damage your overall health.
Other health issues associated with sleep apnea include:
A
- High blood pressure
- Heart disease
- Weight gain
- Metabolic syndrome
- Adult asthma
- Acid reflux
- Daytime sleepiness
- Car accidents
- Memory loss
- Depression
Sleep apnea can cause or worsen life-threatening conditions and should always be taken seriously. If you have sleep apnea, you should pursue proper treatment as soon as possible.
How to Diagnose Sleep Apnea
Sleep apnea is diagnosed through a sleep study, which tracks your breathing while you’re asleep. If you’re experiencing symptoms of sleep apnea, see your doctor to express your concerns.
Sleep Apnea Doctors
The following types of doctors are all capable of diagnosing and/or treating sleep apnea:
- Primary care physician. Your primary care physician will most likely be your first stop. He or she can help with simple advice such as lifestyle changes or, if needed, prescribing medication for nasal congestion. Your PCP can also give you a referral to a specialist if needed.
- ENT. An ear, nose, and throat doctor (also called an otolaryngologist) can help if your airway is naturally narrower. ENTs prescribe CPAP machines.
- Pulmonologist. Pulmonologists treat the lungs and the rest of the respiratory system. They sometimes treat sleep apnea.
- Somnologist. A somnologist, or sleep specialist, is the correct doctor for all things involving sleep. They can advise you on the best ways of treating sleep apnea.
- Neurologist. If you have central sleep apnea, you may need to see a neurologist. He or she can order a sleep study and provide recommendations to help you prevent a stroke (which is more common in sleep apnea patients).
- Dentist. If you’ve already been diagnosed with sleep apnea, a dentist can work together with your other medical doctor to help you find the right mouthpiece or other type of treatment
Sleep Apnea Testing
The most common diagnostic testing for sleep apnea is polysomnography (a sleep study). A sleep specialist will oversee this test. In some cases, your primary care physician may recommend pursuing additional testing from an ENT to check for nasal issues that could cause obstructive sleep apnea, or from a neurologist to look for causes of central sleep apnea.
What is Polysomnography?
Polysomnography is a sleep study that can diagnose sleep apnea (as well as other sleep disorders). While it can be inconvenient, the test is not invasive or painful. The test records things like your brain waves; the oxygen level in your blood; your heart rate; your breathing; and the movements of your eyes and legs while you’re asleep.
Often, sleep studies take place at a hospital or at a sleep center in a room that’s similar to a hotel room. In some cases, you might be able to do the sleep study at home. Home sleep studies don’t have the full capabilities of typical sleep studies, but they’re able to diagnose obstructive sleep apnea.
The sleep study will record your body’s shifts between different phases of “light” sleep and “deep” sleep. To prepare for a sleep study, you’ll likely be asked to avoid alcohol, caffeine, and sedatives during the day leading up to the study. You should also avoid putting on lotion, since you will have sensors on your skin.
If your test is being performed in a hospital or sleep center, you’ll arrive in the early evening with everything you need for the night. A technician will apply electrodes to your skin; for an at-home sleep study, you’ll put the sensors on yourself.
You will then be instructed to go to sleep as usual. Throughout the night, the technician will monitor your brain waves, oxygen level, heart rate, and other vitals using the electrodes, which send data to a computer.
The next morning, you’ll wake up, leave the sleep center, and go about your day as normal. For an at-home study, you will likely need to return the equipment to your doctor’s office. Your doctor will review the results of the sleep study and let you know what the test showed.
Treating sleep Apnea with Lifestyle Changes
Depending on what type of sleep apnea you have and how severe it is, you may be able to treat it through lifestyle changes and home remedies. Speak to your doctor about whether the following lifestyle changes may be helpful for you.
Weight Loss
While anyone can develop sleep apnea, obesity is one of the leading factors that causes sleep apnea. If your doctor recommends losing weight, follow their suggestions to reach a healthier weight. Healthy methods of weight loss include:
- Setting realistic goals
- Eating less refined carbs and cutting out sugary drinks
- Regularly participating in physical exercise
- Plan meals ahead of time and consider working with a dietitian or nutritionist
Losing weight may help treat your sleep apnea.
Avoiding Alcohol
If you drink alcohol or smoke cigarettes, this
may be contributing to your sleep apnea. If you can, stop drinking completely. If not, consider limiting alcohol to only weekends, or drinking earlier in the evening instead of right before bed. You should also stop smoking cigarettes.
Review Your Medications
Certain medications
may cause or worsen sleep apnea. Speak with your doctor about the medications you currently take and if they might be contributing to your condition. Medicines that could impact your sleep and your breathing include:
- Antihistamines (Benadryl, Claratin, Allegra, Zyrtec)
- Benzodiazepines (Xanax, Valium, Ativan)
- Barbiturates
- Opiates (Hydrocodone, Oxycodone, Fentanyl, Morphine, Codeine)
Ask your doctor if it’s safe for you to stop these medications and see if your sleep apnea improves.
Practice Good Sleep Hygiene
Sometimes, the lifestyle changes you need to make could be simple—such as improving your sleep hygiene or sleeping on your side. People who
sleep on their back may snore more often. Try sleeping on your side or stomach so your airways will stay open more easily. You can also improve your sleep quality by sticking to a bedtime routine and avoiding computer or electronic screens before bed. These are simple methods of sleep apnea treatment without CPAP.
Risk Factors for Sleep Apnea
In some cases, you may have factors that place you at a higher risk for sleep apnea. These are generally things you can’t control. For example, you may be more at risk for sleep apnea if you have a family member with obstructive sleep apnea; you are post menopause; or you have Down syndrome. Sleep apnea is also
more common in men than in women, and most common in middle-aged and older adults. While you can’t control your age or your family history, it’s still helpful to know the risk factors for sleep apnea.
Sleep Apnea Therapies
If lifestyle remedies don’t work for you, another common method of treating obstructive sleep apnea or central sleep apnea is through devices such as continuous positive airway pressure (CPAP) or a mouthpiece.
Continuous Positive Airway Pressure (CPAP)
A device called a
continuous positive airway pressure (CPAP) can treat your sleep apnea. Your ENT or sleep specialist can prescribe this device for you through a home healthcare company. The device consists of a mask that goes over your nose (and sometimes your mouth, too). Tubing runs from the mask to a bedside machine.
You’ll put on the mask before you go to sleep each night. Pressurized air flows through the tubing into your airways while you sleep. The flow of air keeps your airway passages open so you won’t stop breathing when you sleep. CPAP machines are a good fit for treating obstructive sleep apnea and treating central sleep apnea.
Benefits of CPAP machines include:
- Higher quality sleep
- Lower risk of heart attack and stroke
- Less daytime sleepiness
Some people may experience side effects such as:
- Nasal congestion
- Dry mouth
- Nosebleeds
- Feelings of claustrophobia
- Skin irritation
- Insomnia
It can take some time to get used to wearing a CPAP, and many of these side effects will improve or go away with time. If you use a CPAP, it’s your responsibility to clean the tubing, mask, and water chamber on a regular basis. Keep in mind that it can also be difficult to travel with a CPAP. Your doctor will be able to advise you on the best treatment options for your medical condition and your lifestyle. Usually, insurance plans will cover at least part of CPAP treatment.
Oral Appliance
In some cases, a doctor may recommend oral appliance therapy instead of continuous positive airway pressure. Your doctor can refer you to a dentist who will create a customized dental device. This oral appliance positions your jaw correctly, advancing the lower jaw, so your airway will stay open. Some appliances may also prevent your tongue from blocking your throat. There are three main types of devices for treating obstructive sleep apnea:
- Mandibular advancement devices. These devices are made of hard plastic that snaps over your teeth. They push your lower jaw forward.
- Snore guards.
Snore guards are another option to reposition your lower jaw.
- Tongue-retaining devices. Tongue-retaining devices are made of a soft plastic that goes around your tongue to keep it out of your airway all night.
To create the oral appliance, your dentist will make an impression of your teeth. Once the device is made, you may need to return for a fitting. When you start using the device every night, you will need to wear a repositioner briefly in the morning to realign your bite. And similar to a CPAP machine, you’ll be responsible for keeping the appliances clean and bacteria-free.
Dental devices for treating obstructive sleep apnea have
several benefits. Unlike CPAPs, they are quiet; they do not require electricity; and they are easy to travel with. However, they can be uncomfortable and come with risks including:
- TMJ pain
- Loose teeth
- Bite changes
- Dry mouth
- Excessive drooling
Dental devices are usually best for mild or moderate sleep apnea. Similar to CPAPs, you can likely expect your insurance company to cover part of the cost.
Surgery for Sleep Apnea
In severe cases, where sleep apnea cannot be treated by lifestyle changes or an assistive device, your doctor may recommend surgery. Surgery might improve or even eliminate your sleep apnea. Common procedures for sleep apnea include nasal surgery; tissue removal; jaw surgery; or soft palate implants.
Nasal Surgery
A
septoplasty straightens your nasal septum (the bone and cartilage separating your nostrils) to make it easier for you to breathe. While this is typically an outpatient procedure, full recovery may take up to three months.
Turbinate reduction addresses the curved bones in your nasal passage, which are called
turbinates. This procedure reduces the size of these bones to open up your airway.
Tissue Removal
This procedure, called
uvulopalatopharyngoplasty, takes out excess tissue in the throat to open the upper airways. Tissue that might be removed includes the uvula; parts of the soft palate; and the tonsils and adenoids. Full recovery
takes 2-3 weeks and comes with a very sore throat.
Maxillomandibular Advancement
This procedure repositions the bones in your jaw, creating more space behind the tongue to open up your airway. Typically, patients need to stay in the hospital for 2-3 nights, although pain is manageable after the procedure. Full recovery takes about six weeks. Maxillomandibular advancement is highly effective for treating sleep apnea:
In one study, this surgery reduced the severity of sleep apnea in all 16 participants by over 50%.
Hyoid Suspension
Your hyoid bone is located below your lower jaw and helps you speak and swallow. In some cases, hyoid suspension—a procedure that moves the hyoid bone to open up your airway—can be helpful. The surgery repositions the hyoid bone to expand your airway and prevent your tongue from falling back in your mouth. While this procedure is somewhat complex, post-procedure pain is very manageable.
Soft Palate Implants
Soft palate implants, also known as the
Pillar Procedure, treat mild cases of sleep apnea. In this procedure, your surgeon takes three small polyester rods and implants them into your soft palate (the back of the roof of your mouth). These rods make your soft palate stiffer, so it won’t relax and block your airway while you sleep. This is a minimally invasive procedure that generally has lasting results.
A Lasting Solution for Sleep Apnea
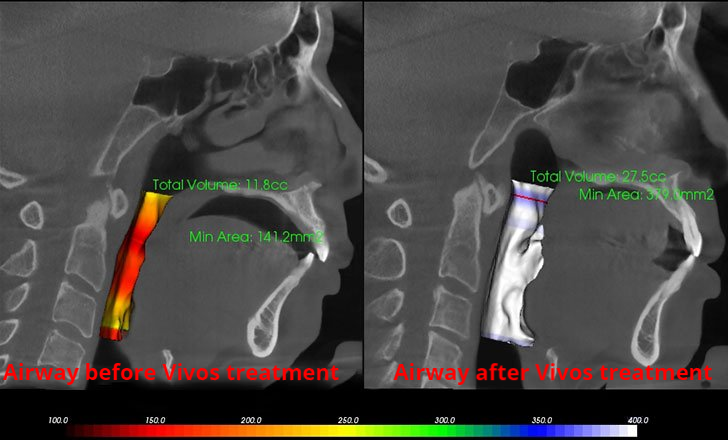
Non-Surgical Cosmetic Enhancements
In addition to its many health benefits, the Vivos appliance is also used for cosmetic correction to a patient’s facial structure for more pleasingly balanced features and a more aesthetic appearance.
Find Out More
Orthodontics Without Braces
Misaligned teeth, an improper bite and other dental issues due to underdeveloped dental arches, can be corrected in both adults and children with the Vivos appliance. Find out more about this application of the Vivos appliance for
adults or
children .
Find Out How the Vivos Appliance Can Help You
Learn if you are a good candidate for the Vivos Biomimetic Oral Appliance. Attend a free educational seminar or request a personal consultation with Dr. Maryam Seifi. Call
(301) 770-1070 or
submit an online request.